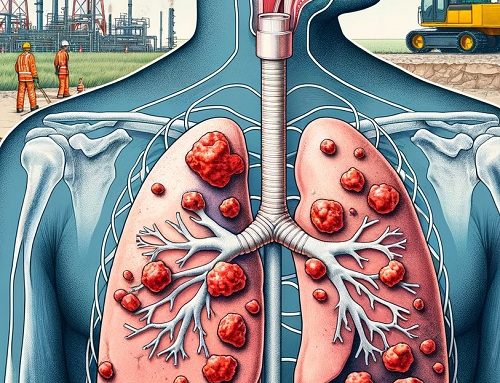
Bloodborne pathogens represent infectious microorganisms in blood that can lead to disease in humans. These include, but aren’t limited to, hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV), which causes AIDS. Workers exposed to these pathogens may face serious or even life-threatening health issues.
Safeguards Provided by OSHA’s Bloodborne Pathogens Standard
All requirements for OSHA’s Bloodborne Pathogens standard can be found in Title 29 of the Code of Federal Regulations at 29 CFR 1910.1030. This standard outlines what employers need to do to protect workers who might be exposed to blood or other potentially infectious materials (OPIM) during their job duties.
In general, the standard mandates that employers:
• Create an exposure control plan: This written plan aims to eliminate or minimize occupational exposures. Employers must develop an exposure determination containing a list of job classifications where all workers have occupational exposure, as well as a list of job classifications where some workers have occupational exposure, and a list of tasks and procedures performed by those workers that result in exposure.
• Update the plan annually: Employers must update the plan yearly to account for changes in tasks, procedures, and positions affecting occupational exposure and technological advancements that eliminate or reduce exposure. Additionally, employers must document in the plan that they have considered and started using appropriate, commercially-available safer medical devices and have sought input from frontline workers in identifying, evaluating, and selecting effective controls.
• Implement universal precautions: Treat all human blood and OPIM as if they’re infectious for bloodborne pathogens.
• Identify and utilize engineering controls: These devices isolate or remove bloodborne pathogen hazards from the workplace, including sharps disposal containers, self-sheathing needles, and safer medical devices like sharps with engineered sharps-injury protection and needleless systems.
• Identify and ensure the use of work practice controls: These practices reduce exposure possibility by altering the way tasks are performed, such as proper handling and disposal of contaminated sharps, specimen handling, laundry handling, and cleaning contaminated surfaces and items.
• Provide personal protective equipment (PPE): Offer equipment like gloves, gowns, eye protection, and masks at no cost to the worker. Employers must clean, repair, and replace this equipment as needed.
• Offer hepatitis B vaccinations: Make these vaccinations available to all workers with occupational exposure within 10 days of initial assignment, after the worker has received the required bloodborne pathogens training.
• Provide post-exposure evaluation and follow-up: Offer these services at no cost to any occupationally exposed worker experiencing an exposure incident, such as specific eye, mouth, other mucous membrane, non-intact skin, or parenteral contact with blood or OPIM. This includes documenting exposure routes and circumstances, identifying and testing the source individual for HBV and HIV infectivity (with consent), collecting and testing the exposed worker’s blood (with consent), offering post-exposure prophylaxis, counseling, and evaluating reported illnesses. Healthcare professionals will provide a limited written opinion to the employer, and all diagnoses must remain confidential.
• Use labels and signs to communicate hazards: Warning labels should be attached to containers of regulated waste, contaminated reusable sharps containers, refrigerators and freezers containing blood or OPIM, other containers storing, transporting, or shipping blood or OPIM, contaminated equipment being shipped or serviced, and bags or containers of contaminated laundry. Red bags or containers can be used as an alternative to labels. In HIV and HBV research laboratories and production facilities, signs must be posted at all access doors when OPIM or infected animals are present.
• Offer information and training to workers: Ensure workers receive regular training covering all elements of the standard, including but not limited to: information on bloodborne pathogens and diseases, methods to control occupational exposure, hepatitis B vaccine, and medical evaluation and post-exposure follow-up procedures. Employers must provide this training during initial assignment, at least annually thereafter, and when new or modified tasks or procedures affect a worker’s occupational exposure. Additionally, HIV and HBV laboratory and production facility workers must receive specialized initial training, along with the training provided to all workers with occupational exposure. Workers should have the opportunity to ask questions during training, which must be presented at an educational level and in a language that workers can understand.
• Maintain worker medical and training records: Employers are also required to maintain a sharps injury log, unless exempt under Part 1904 – Recording and Reporting Occupational Injuries and Illnesses, in Title 29 of the Code of Federal Regulations.
For more information, visit OSHA’s Bloodborne Pathogens and Needlestick Prevention Safety and Health Topics web page at: https://www.osha.gov/bloodborne-pathogens.
References: