Outbreaks of avian influenza, commonly known as bird flu, pose serious risks to the health and safety of workers who handle infected birds or poultry. With highly pathogenic strains like H5N1 leading to high mortality rates in bird populations across multiple states, preventing transmission to humans is paramount. This article will provide an in-depth look at avian influenza, its risks, and the critical precautions workers and employers must take to reduce exposures.
Understanding Avian Influenza
Avian influenza viruses are divided into two categories based on severity: low pathogenic (LPAI) and highly pathogenic (HPAI). While LPAI typically only causes minor illness in birds, HPAI strains are highly infectious and fatal. Neither virus commonly infects humans. However, when transmission to humans occurs, it can cause anything from mild symptoms to severe pneumonia requiring hospitalization. Even though H5N1 does not currently spread easily from person-to-person, it is critical to limit human exposures, as these viruses have the potential to mutate into pandemic strains.
Background on Avian Influenza
The Centers for Disease Control and Prevention (CDC) maintains up-to-date tracking and information on all emerging avian influenza viruses with pandemic potential on their Avian Flu website (www.cdc.gov/flu/avianflu). This site provides both workers and employers the current status of H5N1 across the United States. As of November 2022, commercial flocks across multiple states have experienced outbreaks. While the current risk level for human infection remains low, workers in regular, direct contact with infected birds have an elevated occupational hazard. Understanding and properly implementing protective policies and procedures is vital to reduce transmission.
Symptoms of Avian Flu in Humans
When humans contract avian influenza, symptoms can vary tremendously depending on viral load. Some people may be completely asymptomatic. Milder cases elicit symptoms reminiscent of seasonal influenza like:
- Fever
- Cough
- Sore throat
- Runny or stuffy nose
- General body aches and fatigue
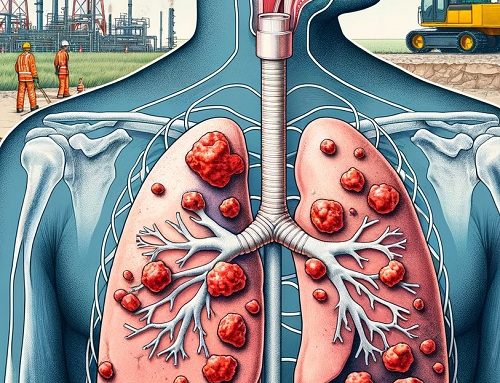
In more severe human cases, people often experience complications like:
- Pneumonia
- Shortness of breath
- Muscle pain
- Headaches
- Diarrhea, nausea, vomiting
- Seizures
A signature symptom of bird flu is lower respiratory involvement (pneumonia). But physicians should not rule out influenza infections even if patients do not present with fever, as many people do not mount one.
How Avian Influenza Spreads to Humans
Human infection almost always occurs via direct exposure to bodily fluids or excretions from infected birds, especially saliva, mucus, and feces. Virus particles can be picked up via:
- Inhalation of aerosolized droplets or dust containing the virus
- Contact between the live virus and eyes, nose, or mouth membranes
- Touching contaminated environmental surfaces then touching the face without properly washing hands first
Understanding transmission routes enables better targeting of safety protocols like personal protective equipment and decontamination procedures.
Employees at Risk of Avian Influenza Exposures
While the average person has extremely low odds of contracting avian flu during an outbreak, several occupational groups endure increased hazard. These include:
Poultry and Commercial Farm Workers Poultry processing, husbandry, and eradication crews endure the highest risks due to their direct, hands-on responsibilities handling infected and dead birds, waste products, and contaminated surfaces. Even workers not directly interacting with flocks can receive exposures via shared on-site transportation, equipment, and facilities.
Animal Handlers
The veterinary field, animal control units, and zookeepers also routinely interact with infected wildlife or treat sick domesticated birds. Appropriate safety steps must be implemented with both routine and emergency veterinary care during outbreaks.
Laboratory Personnel
Microbiologists and clinical laboratory scientists working directly with collected avian influenza virus samples also confront increased exposures from infected tissues or cultures. Diligent adherence to biosafety protocols in the lab is essential.
Healthcare Workers
Physicians, nurses, and other healthcare job functions face hazards treating any patients exhibiting pneumonia symptoms or diagnosed avian flu cases without proper protections in place.
Outbreak Prevention and Response Recommendations
All employees in these higher risk roles have an elevated duty to prevent infections that could occur in their workplace. Here are evidence-based guidelines for employees to follow:
Avoid direct contact with known infected birds whenever possible. Similarly, interacting with potentially contaminated waste items like carcasses, feces, and farm debris should also be avoided.
Practice impeccable hand hygiene before eating or touching the face. Use soap and water for at least 20 seconds. When these are unavailable, alcohol-based hand sanitizers are acceptable substitutes.
Get the seasonal flu shot every year. Even though the vaccine does not cover avian flu strains, preventing co-infection helps avoid dual respiratory illness complications.
Self-isolate at the first sign of any symptoms potentially indicative of influenza — like high fever, cough, difficulty breathing — until definitively ruled out by a physician. Alert supervisors immediately of any illness during outbreaks.
Employers must also uphold several key responsibilities:
Provide employees ample facilities and time for regular, thorough hand washing while working.
- Offer voluntary annual seasonal influenza vaccinations on-site and free of charge.
- Develop clear infection control and isolation protocols should employees exhibit concerning symptoms. Reporting procedures to state/local public health departments must also be established before outbreaks occur.
- Train all potentially exposed staff on hazard awareness, facility procedures, proper personal protective equipment (PPE) usage, and necessary post-exposure precautions. Reinforce training regularly.
- Stockpile sufficient PPE supplies with contingency plans to handle exhausting or damaging stock during extended outbreaks. Track and replace expired equipment and supplies as well.
- Sick leave policies must cover time spent out ill with or awaiting evaluation for influenza-like illnesses per CDC recommendations during outbreak periods.
By jointly committing to optimal infection control practices, both workers and management can collaborate to prevent hazardous avian influenza exposures in high-risk occupational settings even during extensive epidemics.
Appropriate Use of Personal Protective Equipment
For personnel that must have direct physical engagement with known infected birds, properly worn personal protective equipment curtails transmission vectors substantially. Necessary components include:
Gloves and Protective Clothing
Waterproof gloves prevent direct contact between potentially contaminated fluids and the hands. Long water-resistant coveralls, sleeves, aprons, and spats act as the next barrier against particles making skin contact or seeping into regular clothing.
Head and Face Coverings
Hair/beard nets prevent contact with hair that hands frequently touch while working. Non-vented protective eyewear guards against splashes into the mucus membranes. For tasks certain to disturb copious debris or fluids, face shields boost protections from immediate facial areas.
Respiratory Protection
CDC’s guidelines currently require an N95 or equivalent filtration respirator, donned after proper mask fit testing, to protect the lungs from tiny suspended particulate during high exposure tasks like bird eradication or cleanup.
Proper Donning/Doffing Areas & Disposal Stations
To avoid cross-contamination while gearing up, employees should use designated clean spaces for careful stepwise dressing and removal of PPE. Dedicated secure repositories for discarding used contaminated PPE should also be set up to prevent exposure while doffing gear.
Employee training programs must cover proper selection and usage of protective equipment. Supervisors need to monitor staff on an ongoing basis as well to correct any inconsistent compliance with PPE protocols promptly. Facilities must provide necessary cleaning/disinfection stations so employees can refresh PPE when working for extended stints.
Exposure Monitoring & Medical Management Recommendations
In the event of a potential exposure while wearing PPE — or without adequate protection active — specific actions must be taken to protect worker health and stem any further contagion.
- Report the exposure incident to both on-site supervisors and the local or state health department. The latter oversees tracing close contacts and monitoring any emergence of symptoms.
- Regardless of apparent symptom onset, continue checking body temperature at least twice daily for the 10 days post-exposure. Consult healthcare providers for guidance on confirmatory lab testing should fever or early flu signs manifest.
- Avoid contact with other people outside family members already exposed as much as realistically possible while monitoring health. Preventative home isolation curbs community spread. Consider alternative remote work or leave options as well until completing the 10-day surveillance window, if feasible.
- Do not travel outside the local area so that health departments can quickly activate care plans and tracing if disease progression mandates.
- Any employees returning to facilities after infections must be cleared by occupational health following CDC-defined protocols preventing return-to-work too early.
Conscientious monitoring and reporting of potential exposures enables rapid public health containment measures before index cases ignite uncontrolled nosocomial outbreaks in facilities.
Employer Emergency Preparedness Essentials
The scale of responding to large-scale avian influenza outbreaks dictates certain capacity and planning prerequisites employers must address before the crisis burdens worksites.
Stockpiling Equipment and Supplies
Procuring extra caches of PPE, disinfection chemicals, influenza tests, medications, and supplemental housing/services prior to outbreaks enables sustaining operations even if customary supply chain channels collapse in overwhelmed zones.
Coordinating Community Emergency Resources
Develop contacts with nearby healthcare facilities able to accept transfers of severely ill patients, alternative lodging to shelter exposed co-workers, specialized cleaning companies to deploy for contamination events, and government agencies overseeing public advisories and regulatory decisions during outbreaks.
Workforce Training Drills
Practicing components of the avian influenza emergency response plan with employees streamlines adapting policies and procedures when actual events occur. Drilling common potential issues also boosts compliance rates when rapid decisions get made during incidents.
Redundant Communications Platforms
Spreading messages rapidly internally and connecting with response partners relies on multiple communication modalities to account for potential disruptions of any single channel during crises.
Cross-training Personnel
Having facility staff — or contracted temporary workers via staffing agencies — across departments credentialed in procedures like employee exposure evaluation, isolation transport, hazard recognition, equipment decontamination, and workplace sanitization boosts responding resiliency.
Ultimately, the collectively bundled precautions and protocols outlined above offer the best armor workplaces have against elevated biological threats like highly pathogenic H5N1 avian influenza. Staying abreast of the latest protective guidance as outbreaks evolve ensures the safety net around exposed worker populations remains resilient even in dire scenarios. But proper preparation dulls the blades of this particular biologic hazard considerably even under intense conditions. By empowering communities of employees and employers to collaborate around outbreak preparedness and risk reduction, much progress continues getting made advancing workplace readiness – and resilience – for this unique population health challenge confronting essential industries performing critical national infrastructure roles.